When the Past Won’t Let Go: Finding Peace with AI-Supported PTSD Healing
How artificial intelligence is gently guiding trauma survivors toward wholeness
A journey from hypervigilance to hope, where ancient healing wisdom meets modern compassionate technology

Breathe in.
Hold.
Breathe out.
You’re here now. Safe. Present. Yet some part of you remains trapped in that moment—the accident, the violence, the loss, the terror that rewired your nervous system into permanent alert mode.
It’s 3 AM. You’ve jolted awake again, heart racing, sheets damp with sweat. The nightmare was so vivid you can still taste the fear. During the day, ordinary sounds—a door slamming, tires screeching, raised voices—send your body into fight-or-flight mode before your mind can catch up.
This is your reality. This is Post-Traumatic Stress Disorder.
You carry an invisible weight—one that others can’t see but you feel in every hypervigilant glance, every avoided situation, every moment when joy feels impossibly distant. The lifetime prevalence of PTSD among U.S. adults is approximately 7%, but globally, approximately 3.9% of the population experiences PTSD over their lifetime, with dramatically higher rates among veterans, survivors of violence, and those who’ve lived through disasters.
You are not alone. And more importantly—you are not without hope.
What if healing support could meet you precisely where you are, any hour of the day or night, without judgment, without waiting lists, without the barriers that have kept you from help? What if technology, wielded with compassion and wisdom, could become a gentle companion on your healing journey?
This is not about replacing human connection. This is about extending it—using artificial intelligence as a bridge back to wholeness when traditional pathways feel impassable.
Understanding the Terrain: What PTSD Really Does to You
Before exploring how AI can support your healing, let’s honor what you’re experiencing with clear understanding.
Your Nervous System on High Alert
PTSD isn’t weakness. It isn’t failure. It’s your brain’s survival mechanism stuck in overdrive after experiencing something that threatened your safety or sense of self.
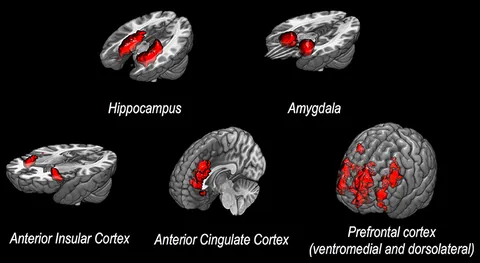
In the neural circuitry model of PTSD, the hypothalamic–pituitary–adrenal (HPA) axis plays a crucial role in stress response and cortisol regulation. The activation of the amygdala, prefrontal cortex, and hippocampus stimulates physiological and psychological changes that once protected you but now create suffering.
What’s actually happening in your body:
Amygdala hyperactivity: Your brain’s threat-detection center remains on high alert, perceiving danger where none exists
Hippocampus changes: Memory processing disrupts, making it hard to distinguish past trauma from present reality
Prefrontal cortex impairment: Your ability to regulate emotions and make calm decisions becomes compromised
HPA axis dysregulation: Stress hormones remain elevated, keeping you in perpetual fight-or-flight mode
This isn’t your fault. This is neurobiological reality—and importantly, neuroplasticity means these patterns can change.
The Symptoms You Know Too Well
Perhaps you recognize yourself in these experiences:
Intrusive memories: Flashbacks that feel like you’re reliving the trauma, nightmares that steal your rest, unbidden thoughts that hijack your day
Avoidance: Steering clear of people, places, conversations, or activities that might trigger memories—even when this shrinks your world
Negative alterations in mood and cognition: Persistent negative beliefs about yourself or the world, emotional numbness, inability to experience positive emotions, memory gaps
Hyperarousal: Constant vigilance, exaggerated startle response, difficulty sleeping, irritability, reckless or self-destructive behavior
These symptoms aren’t character flaws. They’re neurological adaptations that, while once protective, now imprison you in cycles of suffering.
Why Traditional PTSD Treatment Falls Short for So Many
Let’s acknowledge, with compassion and honesty, why you may not have gotten the help you needed—and why this isn’t your fault.
The Gold Standard Treatments
Evidence-based therapies for PTSD are remarkably effective when you can access them:
Cognitive Processing Therapy (CPT): Trauma-focused interventions such as cognitive processing therapy (CPT) have demonstrated short- and long-term effectiveness, helping you examine and challenge unhelpful beliefs about the trauma.
Prolonged Exposure (PE): Gradually and safely confronting trauma memories and avoided situations to reduce their power over you.
Eye Movement Desensitization and Reprocessing (EMDR): Processing traumatic memories while engaging in bilateral stimulation.
These therapies work. The research is clear. But here’s the problem: accessing them isn’t.
The Barriers Between You and Healing
Stigma’s heavy weight: For many—especially veterans, first responders, or those in demanding professional fields—admitting you need help for PTSD feels like admitting weakness. The shame alone keeps millions suffering in silence.
Financial impossibility: Even after gaining access to EBPs, individuals continue to experience significant variability in the quality of services they receive. Quality trauma therapy costs $150-250 per session, often requiring 12-20 sessions or more. Insurance coverage remains inconsistent. For many, effective treatment is simply unaffordable.
Geographic deserts: If you don’t live near a major city, finding a trauma-specialized therapist becomes nearly impossible. Rural areas often have no PTSD specialists within hundreds of miles.
The waiting game: When you finally gather courage to seek help, you’re told the wait list is 3-6 months. During that time, symptoms worsen, hope diminishes, and many give up entirely.
The vulnerability threshold: Sitting across from a stranger, speaking unspeakable experiences aloud—this requires immense courage that not everyone possesses when they’re drowning in symptoms.
Treatment fidelity issues: Research has shown that treatment providers often demonstrate variable treatment competence and tend to deviate from protocol adherence over time. Treatment fidelity may be particularly compromised in the delivery of EBPs for PTSD, as several of these treatments involve encouraging patients to directly confront or discuss trauma memories—a practice that some clinicians may fear is harmful or unduly distressing.
The cruel irony? Those who need help most urgently often face the highest barriers to accessing it.
Where Compassionate Technology Enters: AI as Healing Companion

Here’s what changes when artificial intelligence is developed thoughtfully, ethically, and with trauma survivors’ needs centered:
Not Replacement—Augmentation
Let’s be absolutely clear from the start: AI tools are generally intended to augment, but not replace, existing human-delivered PTSD treatments.
Large language models are not ready to act as stand-alone therapists, but there’s a lot of potential to provide support to humans to improve care for patients.
Think of AI as extending your therapeutic team’s reach into the 168 hours each week when you’re not in session—offering support, teaching skills, providing grounding, and tracking patterns that inform your human-delivered care.
The Four Pathways of AI-Supported PTSD Healing
1. Always-Available Crisis Support
Your trauma doesn’t respect business hours. Flashbacks don’t wait for your Tuesday therapy appointment. Panic attacks strike at 2 AM, when no human therapist is available.
AI-powered tools like Wysa, Woebot, and others provide 24/7 access to evidence-based coping skills. 324 users reported app usage for posttraumatic stress disorder (PTSD) symptoms, fear, and sleep issues. Users identified numerous techniques and spaces offered as being especially helpful, such as physical activity exercises, sleep stories, meditations, cognitive restructuring, and reframing exercises.
When you’re spiraling, you can access:
- Grounding techniques to bring you back to present moment
- Breathing exercises to calm your nervous system
- Cognitive restructuring tools to challenge catastrophic thoughts
- Sleep support when nightmares have stolen your rest
Not as replacements for therapy, but as bridges between sessions—immediate support when you need it most.
2. Personalized Pattern Recognition
Your PTSD triggers are as unique as your fingerprint. Generic advice fails because it ignores your specific constellation of symptoms, triggers, and responses.
Machine learning algorithms were able to discriminate PTSD with an overall accuracy of 0.89. Pooled estimates of classification accuracy from multi-dimensional data (0.96) are higher than single data types (0.86 to 0.90).
AI excels at identifying patterns humans miss, analyzing your data to recognize:
- Specific situations or contexts that trigger symptoms
- Physiological warning signs that precede flashbacks or panic attacks
- Which coping strategies work best for you personally
- Subtle improvements you might not notice yourself, providing encouragement
Over time, your AI companion learns your unique trauma signature and offers increasingly personalized support.
3. Enhanced Therapist Training and Support
The center’s projects include an LLM-based tool to support PTSD therapists as they learn new treatments; a tool to provide support for patients as they complete practice between sessions; a chatbot to help teams develop and execute implementation plans when they adopt new practices; and an LLM-based coach that provides on-demand consultation and support on especially challenging cases.
This addresses a critical gap: not enough trauma therapists, and many who practice don’t maintain high fidelity to evidence-based protocols. AI can help by:
- Providing real-time feedback to therapists during sessions
- Rating treatment fidelity to ensure you’re receiving gold-standard care
- Offering therapists consultation on complex cases
- Supporting training of new trauma specialists
You benefit from better-trained, better-supported therapists—even if you never directly interact with the AI.
4. Between-Session Practice Support
Healing happens between therapy sessions, not just during them. But practicing skills alone at home is challenging without guidance.
One use case involves a therapy partner chatbot that provides support for patients as they complete practice between sessions.
Imagine having a gentle companion that:
- Reminds you to practice your assigned homework
- Guides you through exposure exercises at your own pace
- Provides encouragement when exercises feel overwhelming
- Tracks your progress and reports to your therapist
This continuity of care—previously impossible—dramatically improves treatment outcomes.
Real Tools, Real Support: AI Applications Available Now

These aren’t theoretical future possibilities. They’re tools you can access today.
Wysa: Your 24/7 AI Companion
Wysa is an AI-enabled mental health app that leverages evidence-based cognitive-behavioral therapy (CBT) techniques through its conversational interface (chatbot).
With over 1.3 million users across 30+ countries and 90+ million conversations, Wysa has become one of the most trusted AI mental health companions globally.
What makes Wysa special:
Evidence-based foundation: Built on CBT, Dialectical Behavior Therapy (DBT), and mindfulness principles—the same techniques your human therapist uses
Empathetic responses: High users had significantly higher improvement on depression than low users. 67.7% of user-provided feedback responses found the app experience helpful and encouraging
Comprehensive toolbox: Physical activity exercises, sleep stories, meditations, cognitive restructuring, reframing exercises—all tailored to your needs
Privacy-protected: Anonymous interaction means you can explore your most vulnerable thoughts without fear
Accessibility: Works on low-bandwidth devices, supports multiple languages, adapts to cultural contexts
Real user experience:
“I was feeling really down and I was pleasantly surprised. It was so simple yet so effective. I most definitely recommend it to someone who wants privacy and a healthy listening ear.”
Users appreciate the app’s effectiveness in addressing anxiety, PTSD symptoms, loneliness, and other mental health challenges, with many expressing gratitude for the support it offers.
Woebot: CBT in Your Pocket
An AI-powered chatbot that guides you through the management of distressing thoughts and feelings using principles of Cognitive Behavioral Therapy. Woebot uses natural language processing to understand your responses and adapts its therapeutic approach accordingly.
Particularly helpful for:
- Daily mood tracking
- Identifying cognitive distortions
- Challenging unhelpful thought patterns
- Building consistent self-care routines
NightWare: Disrupting PTSD Nightmares
NightWare is an FDA-cleared digital therapeutic system that uses an Apple Watch to monitor and intervene in PTSD-related nightmares by delivering gentle vibrations to disrupt nightmares without waking the user.
For those whose PTSD manifests primarily in sleep disturbances, this represents a breakthrough—using wearable technology to detect nightmare patterns and gently intervene before they escalate.
Endel: Personalized Soundscapes for Nervous System Regulation
Creates adaptive audio environments based on circadian rhythms, weather, heart rate, and activity. For PTSD sufferers whose nervous systems remain dysregulated, these personalized soundscapes can promote calm, focus, or sleep.
Headspace: Mindfulness for Trauma
While not exclusively for PTSD, Headspace offers specialized meditation and mindfulness content that supports trauma recovery by teaching present-moment awareness and body reconnection.
A Deeper Look: How Omdena Serves Trauma Survivors in Crisis

One organization deserves special attention for its commitment to serving the most vulnerable trauma survivors.
AI for Those the System Forgot
Omdena is a global, collaborative AI platform where data scientists, engineers, and domain experts unite to solve real-world social problems. Their work in PTSD care focuses specifically on populations traditional systems ignore: refugees, war survivors, disaster-affected communities, and those in low-resource environments with no access to formal mental healthcare.
How Omdena’s AI Serves You:
1. Early Detection in Resource-Scarce Settings
Omdena’s AI chatbots identify possible PTSD symptoms by analyzing:
- Emotion patterns in your language
- Linguistic cues that suggest trauma responses
- Self-reported symptoms
- Behavioral indicators
This enables early intervention in areas where trained mental health professionals simply don’t exist—potentially preventing acute stress from becoming chronic PTSD.
2. Culturally Adaptive, Multilingual Support
Unlike generic Western-centric mental health apps, Omdena’s tools:
- Function on low-bandwidth devices and basic smartphones
- Support multiple languages and dialects
- Adapt to cultural contexts and beliefs about mental health
- Work in areas with limited internet connectivity
If you’re a refugee in a camp, a rural villager affected by natural disaster, or anyone in a low-resource environment, Omdena’s AI meets you where you are.
3. Anonymous, Stigma-Free Access
In many cultures and communities, seeking mental health support carries profound stigma. Omdena’s AI chatbot system allows you to:
- Speak anonymously without revealing identity
- Express emotions without judgment
- Discuss trauma safely without face-to-face vulnerability
- Take first steps toward healing without public exposure
This dramatically increases the likelihood that you’ll seek support rather than suffer in isolation.
4. Augmenting Overwhelmed Healthcare Workers
In crisis zones and underserved areas, the few available mental health workers are catastrophically overwhelmed. Omdena’s AI supports them by:
- Filtering high-risk cases requiring immediate human attention
- Automating initial assessments
- Tracking symptom patterns over time
- Highlighting users whose condition is deteriorating
This doesn’t replace human care—it ensures human care reaches those who need it most urgently.
The Stanford Revolution: CREATE Center and the Future of PTSD Care

Funded by an $11.5 million NIH grant, the CREATE Center (Center for Responsible and Effective AI Technology Enhancement of Treatments for PTSD) aims to improve PTSD therapies through responsible AI development, working closely with mental health professionals and survivors to ensure a human-centered approach.
This represents a watershed moment in PTSD care.
What CREATE Is Building for You
Co-directed by Shannon Wiltsey Stirman, a professor of psychiatry and behavioral sciences in the School of Medicine, and Johannes Eichstaedt, a faculty fellow at the Institute for Human-Centered AI, the center focuses on using AI to address post-traumatic stress disorder treatment gaps in the United States.
The four pillars of CREATE’s work:
1. Supporting Therapist Training
An LLM-based tool that helps PTSD therapists learn new treatments more effectively—addressing the shortage of qualified trauma specialists by accelerating training without compromising quality.
2. Between-Session Patient Support
Tools that provide guidance as you complete therapeutic homework, practice exposure exercises, and implement skills learned in therapy—extending your therapist’s support into daily life.
3. Implementation Assistance
A chatbot that helps mental health agencies develop and execute plans for adopting evidence-based practices—removing organizational barriers that prevent you from accessing gold-standard care.
4. Case Consultation Support
An LLM-based coach providing on-demand consultation for especially challenging cases—ensuring even complex trauma presentations receive expert-level care.
The Ethical Foundation
Core to the work will be ensuring these tools are built and deployed responsibly. The research team has already designed frameworks for the evaluation of mental health LLMs.
CREATE’s commitment to responsible AI means:
- Safety protocols that detect concerning distress levels
- Ability to involve human providers when needed
- Transparency about AI limitations
- Engagement with trauma survivors throughout development
- Continuous ethical oversight
This isn’t Silicon Valley moving fast and breaking things. This is careful, ethical, survivor-centered development that prioritizes your safety and wellbeing above all else.
The Evidence Base: What Research Tells Us
Let’s ground this hope in rigorous science.
AI’s Diagnostic Accuracy
A systematic review and meta-analysis analyzing studies found that ML algorithms were able to discriminate PTSD with an overall accuracy of 0.89. This is remarkably high—matching or exceeding human clinical judgment in many contexts.
More impressive still: Pooled estimates of classification accuracy from multi-dimensional data (0.96) are higher than single data types (0.86 to 0.90). ML techniques can effectively classify PTSD and models using multi-dimensional data perform better than those using single data types.
What this means for you: AI can help identify PTSD earlier, distinguish it from other conditions, and predict treatment response—getting you to effective care faster.
Therapy Chatbot Effectiveness
In March 2025, a groundbreaking randomized controlled trial demonstrated that participants with depression experienced a 51% average reduction in symptoms using AI therapy—results mirroring traditional outpatient therapy for certain conditions.
While this study focused on depression rather than PTSD specifically, it validates the broader principle: properly designed AI therapy tools can deliver clinically significant improvements.
Research Momentum Building
A bibliometric analysis reveals a significant increase in publications since 2017. Kerry J. Ressler has emerged as the most influential author in the field to date. The United States leads in the number of publications, producing seven times more papers than Canada, the second-ranked country, and demonstrating substantial influence.
The research community is mobilizing rapidly around AI for PTSD, with interdisciplinary collaboration between clinicians, computer scientists, and ethicists accelerating innovation while maintaining safety.
Your Journey: Integrating AI Support Into PTSD Healing
Let’s make this practical. How might you actually use AI support in your healing journey?
Week 1: Creating Safe Foundation
Day 1-3: Establishing Connection
Download Wysa or another trusted AI mental health app. Don’t expect miracles immediately—simply begin building familiarity.
- Spend 10 minutes daily conversing with the chatbot
- Share one emotion you’re experiencing without censoring yourself
- Try one suggested grounding exercise when triggered
The goal isn’t transformation—it’s establishing that this tool feels safe to you.
Day 4-7: Identifying Patterns
Begin basic tracking:
- What times of day are triggers strongest?
- Which situations consistently activate your nervous system?
- What early warning signs precede flashbacks or panic?
Your AI companion can help you notice patterns you’ve been too close to see.
Week 2: Building Skills Toolbox
Focus: Nervous System Regulation
Each day, practice one technique until it becomes familiar:
Monday: Box breathing (4-4-4-4 pattern)
Tuesday: Progressive muscle relaxation
Wednesday: Grounding through senses (5-4-3-2-1)
Thursday: Body scan meditation
Friday: Bilateral stimulation exercises
Weekend: Review which tools felt most accessible
Your AI app can guide you through each technique, provide timing, and track which ones you find most effective.
Week 3: Gentle Exposure Practice
Working WITH your therapist (if you have one) or preparing for eventual therapy (if you don’t yet):
- Identify one mildly distressing memory (not your most traumatic—start small)
- Use your AI companion to guide brief exposure (1-2 minutes)
- Practice grounding immediately after
- Notice that you can survive remembering and return to present
This builds capacity for eventual trauma processing while maintaining safety.
Week 4: Integration and Reflection
- Review your month’s data with AI companion
- Identify which interventions were most helpful
- Notice any subtle improvements in sleep, anxiety, or functioning
- Set intentions for next month
If you’re working with a therapist, share your AI app data to inform your next session.
Long-term: AI as Part of Your Healing Ecosystem
Not your only tool, but a reliable companion that:
- Catches you when symptoms flare
- Reinforces skills learned in therapy
- Provides objective tracking of your progress
- Offers encouragement when hope wavers
Honoring the Limitations: What AI Cannot and Should Not Do

Despite the advancements in AI and AI’s potential to improve the treatment of PTSD and other mental health concerns, it is critical to take a cautious and phased approach to the use of AI in clinical care.
Where AI Falls Short
Cannot replace therapeutic relationship: Clinicians must be able to interpret AI outputs, monitor for potential errors, and play a key role in developing and maintaining the therapeutic alliance essential to effective treatment.
The healing that happens when another human truly sees you, holds space for your pain, and witnesses your journey—this remains irreplaceable.
Cannot handle crisis situations: Clinical safety must be a top priority. AI systems intended for direct patient use require robust protocols for detecting concerning levels of distress and must have the ability to involve a skilled human provider as needed.
If you’re experiencing suicidal thoughts, actively self-harming, or in acute crisis, you need immediate human intervention, not an AI chatbot.
Cannot work for everyone equally: The applicability of generated models to marginalized communities should also be explicitly tested and validated prior to their implementation.
AI systems trained predominantly on data from certain demographics may not serve everyone equally well. Ongoing work addresses this, but current limitations exist.
Cannot substitute for medical evaluation: Complex PTSD, especially with dissociative features, often requires comprehensive assessment and potentially medication management that only licensed professionals can provide.
The Optimal Integration
Think of your healing as a three-legged stool:
Leg 1: Professional trauma therapy (weekly/bi-weekly) for deep processing, complex skill-building, and treatment planning
Leg 2: AI-powered support (daily/as-needed) for between-session skill practice, crisis management, and pattern tracking
Leg 3: Human community (ongoing) through support groups, trusted friends/family, peer support for accountability and belonging
Remove any leg, and the stool becomes unstable. All three together create solid foundation for healing.
Moving Forward: Your Invitation to Begin
You’ve carried this weight long enough.
The hypervigilance that exhausts you. The nightmares that steal your rest. The triggers that keep you from living fully. The sense that you’ll never be the person you were before the trauma.
You’re right about that last part—you won’t be who you were before. Trauma changes us. But change doesn’t mean diminishment. With support, you can become someone who’s integrated their experience, someone whose strength includes vulnerability, someone who knows darkness but chooses light anyway.
AI support won’t erase your trauma. It won’t make PTSD disappear overnight. It won’t replace the courage required to do this healing work.
But it can meet you where you are, any hour you need support, without judgment, without wait lists, without the barriers that have kept you suffering in isolation.
Starting This Moment
Today, you might:
- Download one trusted AI mental health app (Wysa, Woebot, Headspace)
- Practice three conscious breaths
- Tell the AI chatbot one thing you’re feeling right now
- Complete one grounding exercise
- Research trauma therapists in your area (even if you’re not ready to call yet)
This week, you might:
- Establish a daily check-in practice with your AI companion
- Track your triggers and warning signs for seven days
- Try three different nervous system regulation techniques
- Reach out to one person you trust about your struggle
- Investigate whether your insurance covers trauma therapy
This month, you might:
- Develop a consistent routine with your chosen AI tools
- Make an appointment with a trauma-specialized therapist
- Connect with a PTSD support group (online or in-person)
- Notice subtle shifts—slightly better sleep, moments of genuine calm, reduced avoidance
- Begin to trust that healing, while non-linear, is possible
The Path Isn’t Linear
Some days will feel like backward movement. Symptoms will flare. You’ll question whether anything is working. This is normal. This is part of healing.
Your AI companion can help you see the bigger picture—tracking trends you’re too close to notice, providing encouragement when you’re drowning in a bad week, reminding you of progress you’ve already made.
But the fundamental work is yours. The courage to keep showing up. The willingness to feel what you’ve been avoiding. The choice to believe, even when belief feels impossible, that you deserve peace.
The Larger Vision: A World Where Trauma Survivors Don’t Suffer Alone

Many mental health agencies don’t have the resources to support their staff and get trained on new treatments, which means patients don’t have the help they need.
Imagine a different world:
Where every trauma survivor, regardless of location, finances, or circumstances, has immediate access to evidence-based support.
Where stigma doesn’t prevent you from seeking help because your first steps can be anonymous and private.
Where therapists have AI tools that make them more effective, more supported, and less burned out.
Where PTSD is caught early, before acute stress becomes chronic disorder.
Where healing isn’t a privilege of the wealthy and well-connected but a right accessible to all.
This is the promise of responsibly developed, ethically deployed AI in trauma care—not a distant fantasy but an emerging reality being built by dedicated researchers, compassionate technologists, and trauma survivors themselves.
Key Takeaways
- PTSD is a neurobiological condition, not weakness—resulting from changes in brain regions that regulate threat response, emotion, and memory
- 7% of U.S. adults and 3.9% globally experience PTSD in their lifetime, with higher rates among veterans, survivors of violence, and disaster-affected populations
- Traditional barriers (stigma, cost, geography, wait times) prevent most trauma survivors from accessing evidence-based care
- AI augments, never replaces human trauma therapy—extending therapeutic support into the 168 hours between sessions
- Multiple validated tools exist now: Wysa (324 users report PTSD support), Woebot, NightWare (FDA-cleared), and others provide accessible support
- Machine learning achieves 89% accuracy in identifying PTSD, with multi-dimensional data reaching 96% accuracy
- Stanford’s CREATE Center ($11.5M NIH-funded) is developing responsible AI tools for therapist training, patient support, and case consultation
- Omdena serves vulnerable populations: Refugees, disaster survivors, and those in low-resource settings often ignored by traditional systems
- Safety and ethics are paramount: Proper AI systems detect distress, involve human providers when needed, and undergo rigorous evaluation
- Optimal healing combines three elements: Professional trauma therapy, AI-powered daily support, and human community—no single element alone is sufficient
Research Studies & Resources Referenced
Key Clinical and Review Studies:
- CREATE Center Launch (2025) – Stanford University. “New center poised to advance AI innovation in PTSD treatment.” Stanford Report, August 2025. Stanford News
- Generative AI in PTSD Treatment (2025) – Held, P., et al. “Generative artificial intelligence in posttraumatic stress disorder treatment: Exploring five different use cases.” Journal of Traumatic Stress, 2025. PMC12551617
- Machine Learning for PTSD Access (2025) – Published in British Journal of Clinical Psychology. “Using machine learning to increase access to and engagement with trauma-focused interventions for posttraumatic stress disorder.” PMC11797152
- Current Status and Future Directions (2025) – “Current Status and Future Directions of Artificial Intelligence in Post-Traumatic Stress Disorder: A Literature Measurement Analysis.” Behavioral Sciences, 15(1):27. MDPI
- Responsible AI Framework (2025) – Stade, E.C., et al. “Readiness evaluation for artificial intelligence-mental health deployment and implementation (READI): A Review and proposed framework.” Technology, Mind, and Behavior, 6(2). Stanford
- Large Language Models Proposal (2024) – Stade, E.C., et al. “Large language models could change the future of behavioral healthcare: a proposal for responsible development and evaluation.” NPJ Mental Health Research, 3(1):12. Nature
- Systematic Review and Meta-Analysis (2024) – “The application of machine learning techniques in posttraumatic stress disorder: a systematic review and meta-analysis.” npj Digital Medicine. Nature
- Therapeutic Communication Comparison (2025) – Scholich, T., et al. “A comparison of responses from human therapists and large language model-based chatbots to assess therapeutic communication: Mixed methods study.” JMIR Mental Health, 12:e69709. [JMIR](https://doi.org/10.






