How AI saved me from one of 5 SINS : Gluttony
When food becomes a battle, technology offers a gentle path to reconciliation
Discovering harmony between ancient mindfulness practices and modern artificial intelligence

Breathe.
You’re standing in front of your open refrigerator at 11 PM. Again. Your heart races. Your mind swirls with thoughts—I shouldn’t. But I need to. Just this once. Tomorrow I’ll be better.
The familiar pull is there, magnetic and insistent. The phone in your pocket buzzes gently. A notification from your app: “Pause. Notice what you’re feeling right now. Are you physically hungry, or is something else calling for attention?”
You close the refrigerator door. Not because someone told you to. But because, for the first time in months, you were given space to choose.
This is not willpower. This is not another diet plan disguised as wellness. This is the quiet revolution happening when artificial intelligence meets the ancient practice of mindfulness—creating pathways to healing that honor both your humanity and your need for support.
The Silent Struggle: Understanding Disordered Eating with Compassion

Before exploring solutions, let’s create space to understand what you may be experiencing without judgment.
What Disordered Eating Really Looks Like
Disordered eating exists on a spectrum. You don’t need a formal diagnosis to be suffering. You don’t need to hit “rock bottom” to deserve support.
Perhaps you recognize yourself in these patterns:
Binge eating: Consuming large amounts of food quickly, often in secret, followed by overwhelming shame and self-criticism. The lifetime prevalence of binge eating disorder (BED) in adults is approximately 1.4%, but countless others experience binge episodes without meeting full diagnostic criteria.
Bulimia: Cycles of binging followed by compensatory behaviors—purging, excessive exercise, or fasting. Adult lifetime prevalence estimates for bulimia nervosa (BN) are approximately 0.8%, yet the suffering extends far beyond these statistics.
Emotional eating: Using food to soothe, numb, or manage feelings rather than responding to physical hunger. This is perhaps the most common and least discussed pattern—affecting millions who would never consider themselves as having an “eating problem.”
Restriction and rigidity: Strict food rules, intense fear of certain foods, or compulsive “clean eating” that actually disconnects you from your body’s natural wisdom.
The Deeper Truth: It’s Never Just About Food
Here’s what the research reveals and what you may already know in your bones: eating disorders are fundamentally about emotional regulation and disconnection from your body’s signals.
Mindfulness-based interventions have demonstrated medium-large to large effects in reducing binge eating, precisely because they address this core issue: the inability to sit with difficult emotions without seeking escape through food.
When you feel overwhelmed, anxious, lonely, or even joyful, your nervous system seeks comfort. For complex neurological and psychological reasons, food became your refuge. There is no shame in this. Your body was trying to protect you.
The challenge? What once served as protection now creates its own suffering—physical discomfort, emotional shame, social isolation, health consequences, and a persistent sense of being trapped in patterns you can’t control.
Why Traditional Approaches Often Miss the Mark
Let’s acknowledge, with compassion, why you may have tried many things before arriving at this article—and why they may not have worked.
The Diet Culture Trap
Most eating disorder treatment happens in a culture that simultaneously:
- Pathologizes binge eating while normalizing restriction
- Promotes “wellness” that’s actually disordered eating in disguise
- Offers solutions that increase disconnection from your body
You’re told to control your eating through:
- Meal plans that ignore your hunger cues
- Food rules that create more anxiety
- Willpower rhetoric that blames you for “failing”
This isn’t treatment. This is more of what created the problem in the first place.
The Access Problem
Even when you seek evidence-based help like Cognitive Behavioral Therapy (CBT) or Dialectical Behavior Therapy (DBT), you encounter barriers:
Limited availability: Only 30% of patients achieve full remission from binge eating with standard CBT, and accessing quality treatment requires resources many don’t have.
Cost prohibitions: Specialized eating disorder therapy often costs $150-300 per session, with insurance covering limited visits—if at all.
Waiting lists: Months-long waits for treatment slots, during which your relationship with food continues to deteriorate.
Shame and stigma: The vulnerability required to reach out is immense. For many, the threshold feels insurmountable.
The Missing Piece: Moment-to-Moment Support
Traditional therapy offers valuable insights during weekly sessions. But eating decisions happen multiple times daily, in real moments when you’re alone with your thoughts, your kitchen, and your pain.
What if you had support precisely when and where you needed it most?
Where AI Meets Mindfulness: A New Path Forward

Let’s be clear from the beginning: Artificial intelligence has the potential to revolutionize eating disorder research, treatment, and practice by assisting with complex problems such as predicting illness prognosis, supporting diagnostic decisions, and tailoring treatment plans.
AI is not here to replace human connection, therapeutic relationships, or the wisdom of trained professionals. Rather, it extends their reach—offering you continuous, personalized support that adapts to your unique patterns.
The Four Pillars of AI-Enhanced Mindful Eating
1. Real-Time Awareness Cultivation
Traditional mindfulness teaches presence. AI helps you practice it when it matters most.
When patterns in your data suggest you’re entering a high-risk time—perhaps evening hours when you typically struggle, or days when stress levels spike—your AI companion gently reminds you to pause.
Not to control. But to notice.
“Before opening that food delivery app, let’s check in. What sensations do you notice in your body right now? What emotions are present?”
This isn’t restriction. It’s creating space between urge and action—the space where choice lives.
How it actually works:
Smartphones are being integrated into traditional treatment frameworks, allowing patients to log emotions and behaviors in real-time, enabling more targeted therapeutic discussions.
Your AI tool learns your unique patterns by tracking:
- Time of day and associated mood states
- Situational triggers (stress at work, conflict with loved ones, boredom)
- Physical hunger versus emotional hunger cues
- Behaviors that precede binge episodes
With this understanding, it can offer tailored prompts that support interoceptive awareness—knowing when you’re genuinely hungry versus eating for other reasons.
2. Compassionate Emotional Support
Imagine having a gentle, non-judgmental presence available 24/7 when shame spirals threaten to overwhelm you.
Generative AI chatbots could aid humans in offering consistently high levels of support and empathy in patient-facing interactions.
When you’ve just experienced a binge episode—when self-criticism is loudest—your AI companion responds with techniques from Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT):
“I notice you’re experiencing difficult emotions right now. Let’s practice the STOP skill together:
- S: Stop. Pause.
- T: Take a breath.
- O: Observe what you’re feeling without judgment.
- P: Proceed mindfully with what you need.”
It doesn’t shame. It doesn’t lecture. It holds space.
The therapeutic foundation:
DBT consists of four structural elements focused on mindfulness (the core skill), emotion regulation, distress tolerance, and interpersonal effectiveness—particularly effective for eating disorders because disordered behaviors often become ways to deal with upsetting feelings.
AI tools deliver these evidence-based techniques when you need them, not just during weekly therapy appointments.
3. Personalized Pattern Recognition
Your relationship with food is as unique as your fingerprint. Generic advice—”eat three meals daily,” “avoid keeping sweets at home”—fails because it ignores your specific triggers and needs.
AI excels at identifying patterns humans miss.
Over time, your digital companion recognizes that:
- Your binge episodes cluster on Sunday evenings (anticipatory anxiety about the work week?)
- They increase during weeks when you skip your morning walk (movement as emotional regulation?)
- They decrease when you’ve had meaningful social connection (loneliness as trigger?)
- Specific foods aren’t the issue—it’s the thoughts you have about those foods that activate shame spirals
Armed with these insights, your AI tool offers personalized interventions:
“I’ve noticed you’re ordering delivery for the third time this week, and it’s Wednesday evening—typically a vulnerable time for you. Would it help to try a 5-minute grounding exercise before deciding? Or would you like to explore what’s feeling heavy right now?”
The technology at work:
Machine learning models based on physiological signals from wearable devices can predict eating disorder behaviors with up to 90% accuracy, enabling preventive rather than reactive support.
4. Integration with Professional Care
The most sophisticated approach combines AI support with human expertise.
Emerging hybrid models of care utilize smartphone data to inform clinician action, where real-time passive and active data streams can alert providers to concerning patterns.
Your therapist receives aggregated insights (with your permission):
- Frequency of binge episodes over the past month
- Emotional patterns that precede problematic eating
- Which coping strategies you’ve tried and how effectively
- Progress indicators showing movement toward healing
This transforms your weekly therapy from “How was your week?” (which you might struggle to remember or articulate) to targeted, data-informed discussions addressing your actual patterns.
The Research Speaks: Evidence for AI-Enhanced Treatment
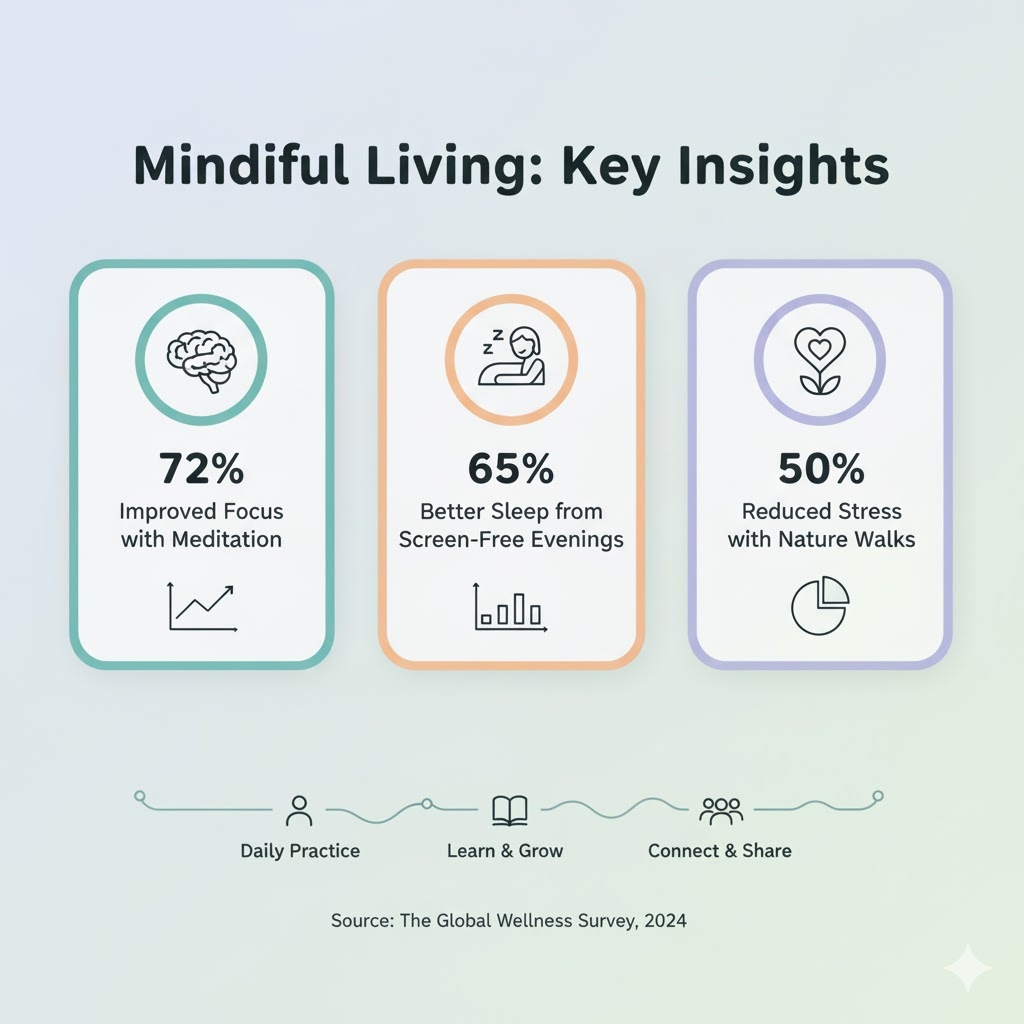
This isn’t experimental or unproven. The evidence base is growing rapidly:
Effectiveness Data
A randomized clinical trial found that app-based CBT-I is effective in preventing the future onset of major depression and improving outcomes among youth with eating concerns and subclinical depression.
Mindfulness-based cognitive therapy (MBCT) significantly improved mindfulness scores, eating behaviors, and reduced the cognitive load of stressful cues related to body shape, weight, and food in patients with BN or BED.
An updated systematic review analyzing 54 studies found that mindfulness-based interventions continued to demonstrate large or medium-large effects in reducing binge eating, with DBT showing particularly strong results.
Accessibility and Engagement
With global rates of smartphone ownership now approaching 90%, the scalability of smartphone tools is impressive, with surveys indicating that some individuals express preference for digital tools over traditional face-to-face options, particularly for managing symptoms and tracking progress outside of formal therapy.
This matters enormously. Technology democratizes access to evidence-based support that was previously available only to those with significant financial resources and geographic proximity to specialized treatment centers.
Clinical Integration
Research shows growing interest and openness among both clinicians and patients toward integrating AI tools as adjuncts to traditional treatment, recognizing that technology enhances rather than replaces therapeutic relationships.
Practical Applications: How AI Supports Your Journey
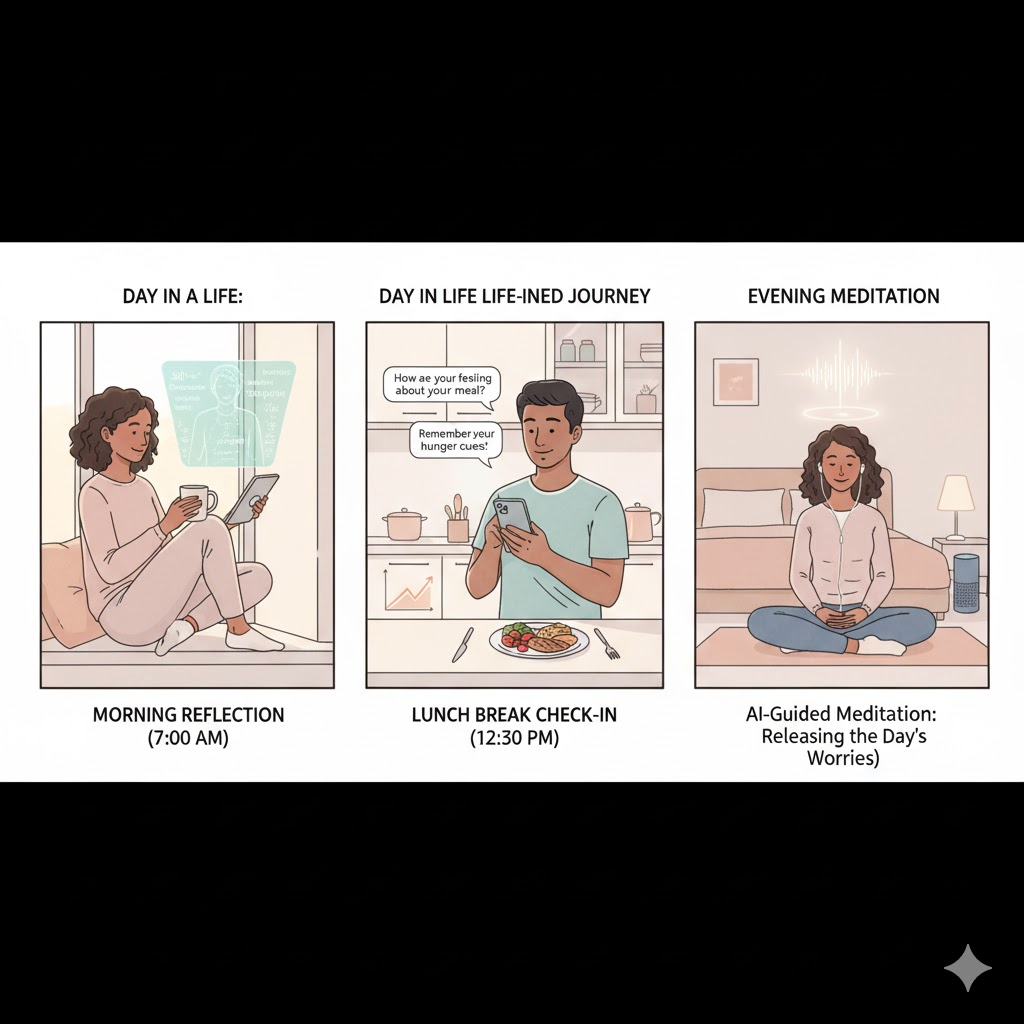
Let’s make this concrete. Here’s how AI-powered mindful eating support manifests in your actual life:
Morning: Setting Intentions
Your phone gently wakes you. Before scrolling social media, your AI companion invites you into presence:
“Good morning. Let’s start with three conscious breaths together. What word or intention would serve you today?”
You choose “gentleness” and type it in. The app adjusts its tone for the day accordingly, knowing you need extra softness today.
Based on your previous patterns, it knows Tuesday mornings are when you’re most likely to skip breakfast (leading to afternoon vulnerability). It suggests a simple prompt:
“What small, nourishing thing sounds good to your body right now? No rules. Just curiosity.”
Midday: Navigating Triggers
You have a difficult meeting. Your stress level spikes. The app (if using wearable integration) notices your elevated heart rate and sends a gentle check-in an hour later:
“I noticed some intensity earlier. How are you feeling now?”
You respond honestly: “Frustrated and want to order everything on the menu.”
Instead of judgment or “don’t do it” rhetoric, the app offers tools:
“That makes complete sense. Your nervous system experienced stress and is seeking regulation. Let’s practice the TIPP skill before deciding:
- Temperature: splash cold water on your face
- Intense exercise: 2 minutes of movement
- Paced breathing: box breathing together
- Paired muscle relaxation: progressive tension release
After we try these, you’ll have more information about what you actually need.”
This isn’t restriction. This is giving your body alternative pathways to regulation that don’t involve food.
Afternoon: Food Order Safeguards
You open your favorite food delivery app. Because you’ve given the AI tool permission to monitor your app usage patterns, it notices and intervenes compassionately:
“I see you’re on the delivery app. Let’s pause together. This is the third time this week during afternoon hours—a pattern we’ve been exploring.
Before ordering, would you be willing to try a 3-minute mindful eating reflection? Or would you prefer to journal briefly about what you’re experiencing?”
Again, not control. Choice.
If you proceed with ordering, the app doesn’t shame you. It asks:
“What would feel genuinely satisfying right now? If you could eat with full permission and presence, what would that look like?”
This question alone shifts you from frantic “forbidden foods” thinking to discernment about what you actually want.
Evening: Processing the Day
During your typical high-risk time—the evening hours when loneliness or fatigue typically trigger urges—your AI companion offers structured support:
“Evening check-in time. Would you like to:
- Practice a body scan meditation (10 minutes)
- Do a written reflection on today’s challenges and victories
- Try a guided eating meditation with your dinner
- Call your designated support person
- Access your list of non-food coping strategies”
You choose the body scan. As you lie on your couch, the app guides you through noticing physical sensations without judgment.
Afterward, it invites reflection:
“What did you notice? What does your body need right now—physically, emotionally, or spiritually?”
Night: Logging Without Shame
Before sleep, the app invites you to log your day. But unlike traditional food diaries that focus on what and how much you ate, this focuses on:
- Emotional experiences throughout the day
- Moments when you practiced mindfulness successfully
- Times when urges arose and how you responded
- What you’re learning about your patterns
- What you want to remember for tomorrow
The AI analyzes this data not to judge, but to identify trends that inform tomorrow’s support.
The Human + AI Partnership: Why You Still Need People

Let’s address what AI cannot and should not do:
What AI Cannot Replace
Therapeutic relationships: The healing power of being truly seen by another human being—feeling their presence, their attunement, their compassionate witnessing of your pain—cannot be replicated by algorithms.
Professional clinical assessment: Complex eating disorders often involve medical complications, co-occurring mental health conditions, and trauma histories requiring expert evaluation.
Accountability and community: Recovery happens in relationship. Support groups, treatment teams, and connections with others who understand your struggle provide irreplaceable elements of healing.
Nuanced emotional attunement: While AI can offer consistently high levels of support, successful implementation requires understanding facilitators and barriers specific to eating disorder populations, which human clinicians navigate with lived wisdom.
The Optimal Integration
The most effective approach combines:
- Professional therapy (weekly or bi-weekly) for deep processing, skill-building, and treatment planning
- AI-powered daily support for real-time guidance, pattern tracking, and moment-to-moment mindfulness
- Human community through support groups, trusted friends, or family for accountability and belonging
- Medical oversight when physical health concerns require attention
Think of AI as extending your therapeutic team’s reach into the 168 hours each week when you’re not sitting in their office—filling a gap that has always existed in traditional treatment models.
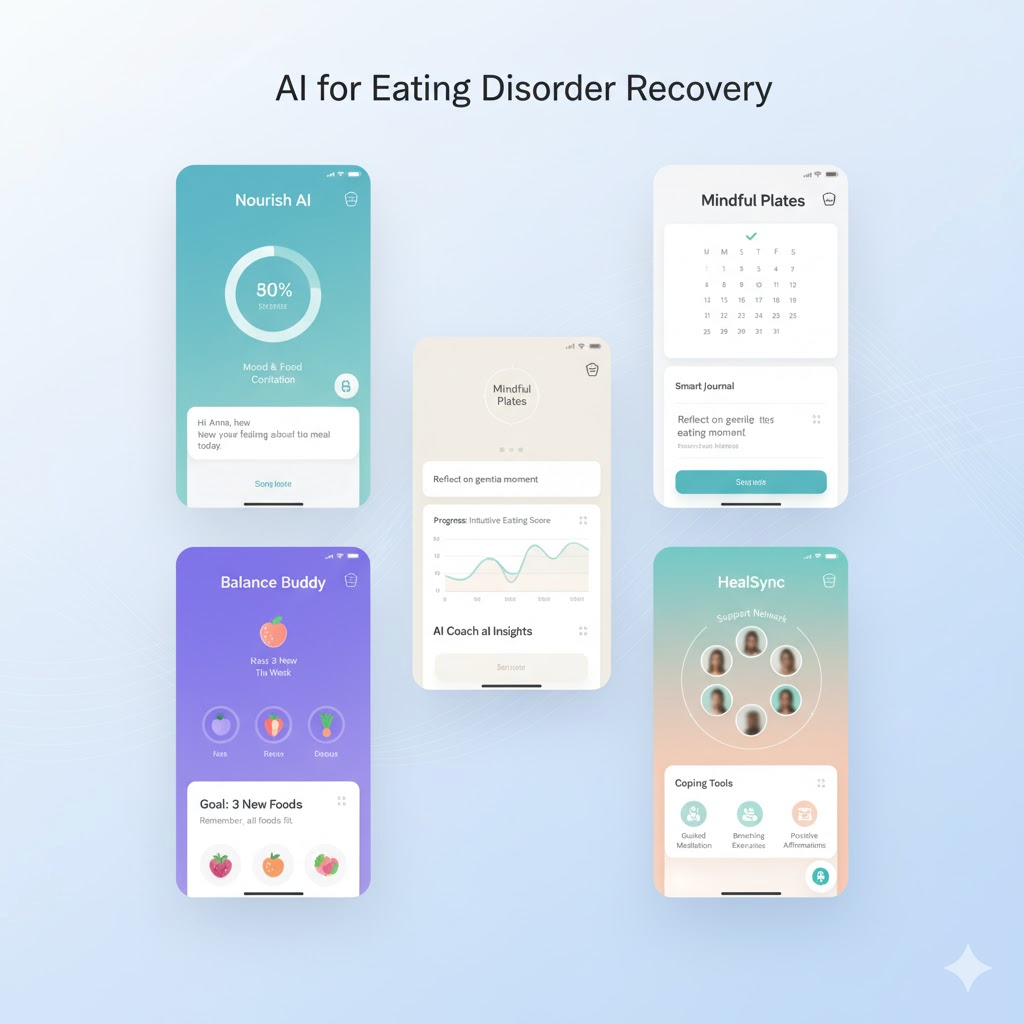
Current AI Tools Supporting Mindful Eating
While this isn’t an exhaustive list, these tools represent the current landscape of AI-enhanced eating disorder support:
Recovery Record
Widely used app combining self-monitoring, meal logging, and AI-driven insights. Recovery Record has been paired with wearable devices like Apple Watches to collect passive physiological and behavioral data, with promising pilot results.
Best for: Those wanting comprehensive tracking with therapist integration options.
Rise Up + Recover
Combines community support with AI-powered meal planning and gentle accountability features.
Best for: Those who benefit from peer connection alongside digital tools.
Nourishly (formerly Eat Right Now)
Uses mindfulness-based eating awareness training with AI-adaptive content based on your progress and patterns.
Best for: Those specifically seeking mindfulness-centered approaches to binge eating.
Betterhelp/Talkspace with Specialized ED Therapists
While primarily human-delivered therapy, these platforms increasingly incorporate AI for matching you with appropriate therapists and providing between-session support.
Best for: Those seeking professional therapy with digital convenience.
Personalized AI Chatbots
Emerging research on generative AI therapy chatbots shows promise for depression, anxiety, and eating disorder symptom treatment, though these tools are still developing.
A word of caution: Not all AI wellness apps are created equally—some pose health risks through inaccurate information or advice. Always vet tools through professional recommendations when possible.
Creating Your Own AI-Enhanced Mindful Eating Practice

Whether or not you use dedicated eating disorder apps, you can integrate AI support into your healing journey.
Step 1: Cultivate Awareness Without Judgment
Begin by simply noticing patterns without trying to change them. Use voice notes, journaling apps, or simple tracking tools to record:
- Times of day when urges are strongest
- Emotions present before, during, and after eating episodes
- Environmental triggers (alone vs. with others, certain locations)
- Physical sensations of hunger versus emotional hunger
Many AI note-taking apps (like Notion with AI, or voice-to-text tools with analysis features) can help identify patterns you might miss.
Step 2: Establish Mindful Check-In Rituals
Set multiple daily reminders on your phone—not to control eating, but to practice presence:
- Morning intention setting
- Pre-meal gratitude or three breaths
- Afternoon emotional check-in
- Evening reflection
Use AI assistants to craft these reminders in language that soothes rather than triggers you.
Step 3: Build Your Digital Toolbox
Create easily accessible resources for high-risk moments:
In your phone’s notes app, store:
- Grounding techniques that work for you
- List of non-food coping strategies
- Affirmations that counter shame spirals
- Contact info for support people
- Evidence of your progress (screenshots of proud moments)
Use AI to enhance these:
- Ask ChatGPT or similar tools to generate personalized affirmations
- Use AI meditation apps for guided practices
- Employ mood-tracking apps that use AI to identify emotional patterns
Step 4: Practice “Pause and Choose”
The fundamental skill in eating disorder recovery is creating space between urge and action.
Use your phone’s timer or meditation apps to practice:
- STOP skill (Stop, Take a breath, Observe, Proceed mindfully)
- Urge surfing (riding the wave of desire without acting)
- Body scans to reconnect with physical sensations
- 5-4-3-2-1 grounding (5 things you see, 4 you hear, 3 you touch, 2 you smell, 1 you taste)
The act of physically engaging with your phone to access these tools creates a mechanical pause—a moment where different choices become possible.
Step 5: Integrate with Professional Support
If you’re working with a therapist, discuss how digital tools might enhance your treatment:
- Share your tracking data to inform sessions
- Ask if they recommend specific apps
- Explore whether they offer text check-ins between sessions
- Discuss using AI tools to practice skills they’re teaching
Research shows that AI technology has yet to be widely integrated into clinical practice for eating disorders, so you may need to educate your provider about available tools—approaching this collaboratively rather than as replacement for their expertise.
The Deeper Invitation: Technology as Gateway to Embodiment
Here’s the paradox: we’re using technology—something often blamed for disconnecting us from our bodies—to facilitate reconnection with our physical selves.
But this makes sense when understood correctly.
The Bridge Back to Your Body
Eating disorders thrive in dissociation—disconnection from bodily sensations, emotions, and needs. You’ve been living in your head, at war with your body, for so long that you’ve lost the ability to hear its wisdom.
AI tools, when used wisely, serve as training wheels for interoceptive awareness. They help you:
Notice what you’re feeling (emotion identification)
Name it without judgment (reducing shame)
Nurture yourself through it (building new neural pathways)
Over time, with practice, you internalize these skills. The external prompts from your app become internal prompts from your own mindful awareness. The AI becomes unnecessary—not because it failed, but because it succeeded in teaching you to listen to yourself again.
The Mindfulness Foundation
Mindfulness-based cognitive therapy works by reducing the cognitive load of stressful cues related to body shape, weight, and food—essentially freeing up mental space currently consumed by obsessive thoughts about eating.
This creates room for:
- Experiencing emotions without immediately reacting
- Noticing body sensations with curiosity rather than fear
- Responding to actual needs rather than conditioned patterns
- Building tolerance for discomfort without seeking food-based escape
From Control to Compassion
The ultimate goal isn’t controlling your eating through better tools—digital or otherwise. It’s developing such deep self-compassion and body trust that external control becomes irrelevant.
You eat when hungry. You stop when satisfied. You savor foods you love without guilt. You notice emotions without needing to change them immediately. You trust your body’s wisdom.
AI tools support this journey not by providing more rules, but by offering gentle guidance back to presence when you’ve drifted into the trance of disordered patterns.
Addressing Concerns and Moving Forward Mindfully

You may have reservations about using AI for something as personal and vulnerable as eating disorder recovery. Let’s honor those concerns.
“Won’t this create more obsession with tracking and monitoring?”
Valid concern. The key is intention and implementation.
Problematic tracking: Calorie counting, weight obsession, rigid food rules disguised as “wellness data”
Healing-oriented tracking: Emotional patterns, mindfulness practice consistency, moments of successful coping, progress indicators
Choose tools that focus on psychological and emotional patterns rather than food quantities or body measurements.
“Can an app really understand my unique situation?”
Not completely. But an advanced AI platform enables personalized treatment by analyzing individual patterns and adjusting interventions accordingly.
The sophistication lies in pattern recognition across thousands of data points you provide—identifying connections you might miss while honoring that your journey is uniquely yours.
“I’m afraid of becoming dependent on technology.”
Again, valid. The intention isn’t lifelong dependence but scaffolded support during your healing process.
Think of AI tools like crutches after an injury—helpful temporarily while you rebuild strength, eventually set aside as you walk independently again.
“What about privacy and data security?”
Critical consideration. Before using any mental health app:
- Review privacy policies carefully
- Understand how your data is stored and used
- Choose tools with strong encryption and HIPAA compliance when possible
- Avoid apps that sell user data to third parties
Ethical considerations and privacy concerns are significant barriers that must be addressed for successful AI implementation in eating disorder care.
“Will insurance cover these tools?”
Currently, most standalone apps aren’t covered, though this is changing as digital therapeutics gain recognition. However:
- Many have free versions with core features
- Some therapists integrate app-based tools into covered treatment
- The cost ($5-30/month typically) is often less than a single therapy copay
View this as an investment in your wellbeing—potentially reducing overall treatment costs by enhancing efficacy and preventing relapse.
Your Invitation to Begin

You’ve carried this burden long enough. The shame, the secrecy, the exhausting mental loops, the physical discomfort, the sense that you’re broken beyond repair.
You’re not broken. You’re human.
Your eating patterns—however chaotic or painful they feel—made sense as survival strategies at some point. They protected you when you had no other tools.
Now, you’re ready for new tools. Gentler approaches. Support that meets you where you are without judgment.
AI-enhanced mindful eating isn’t a magic solution. It won’t instantly dissolve years of conditioning. You’ll still have difficult days. You’ll still need human support and professional guidance.
But it offers something precious: consistent, personalized support in the moments when you’re most vulnerable. A gentle voice reminding you that you have choices. Data that helps you understand yourself more deeply. Skills delivered precisely when you need them.
Starting Small, Starting Now
You don’t need to download ten apps, sign up for therapy, and completely overhaul your life today.
Just begin.
Today, you might:
- Take three conscious breaths before your next meal
- Download one recommended app and explore it with curiosity
- Set a single daily reminder: “Pause. Notice. Choose.”
- Send an email to a therapist you’ve been considering contacting
- Tell one trusted person about your struggle
This week, you might:
- Practice one grounding technique daily
- Track your emotional patterns for seven days without trying to change anything
- Explore which AI tools resonate with your needs
- Make one appointment (therapy, nutritionist, doctor)
- Read more about mindfulness-based approaches to eating disorders
This month, you might:
- Establish a consistent practice using your chosen tools
- Begin integrating mindfulness into mealtimes
- Build your digital toolbox of coping strategies
- Connect with online or in-person support community
- Notice subtle shifts in your relationship with food and your body
The Path Forward
Recovery isn’t linear. You won’t do it perfectly. There will be setbacks, moments of shame, days when you feel like you’ve lost all progress.
But each time you pause, each time you choose presence over autopilot, each time you meet yourself with compassion rather than criticism—you’re rewiring your brain. You’re healing.
The ancient practice of mindfulness teaches us: Be here now. Notice without judgment. Respond with kindness.
Modern AI technology extends this teaching into every moment of your day, every vulnerable hour, every challenging situation.
Together—mindfulness and technology, ancient wisdom and modern innovation, your commitment and digital support—they create a path forward.
Not toward perfect eating. Toward peace.
Not toward control. Toward trust.
Not toward fixing yourself. Toward remembering you were never broken.
Key Takeaways
- Eating disorders are fundamentally about emotional regulation, not just food—explaining why mindfulness-based approaches are so effective
- AI extends therapeutic support into the 168 hours per week when you’re not in therapy, offering real-time guidance at vulnerable moments
- Research validates effectiveness: Mindfulness-based interventions demonstrate large effects in reducing binge eating, with AI enhancing personalization and accessibility
- Four key AI applications: Real-time awareness cultivation, compassionate emotional support, personalized pattern recognition, and integration with professional care
- 90% smartphone ownership makes AI-powered tools remarkably scalable and accessible compared to traditional treatment
- The goal isn’t dependence on technology but using AI as temporary scaffolding while rebuilding body trust and interoceptive awareness
- Human connection remains essential: AI augments, never replaces, therapeutic relationships, professional assessment, and community support
- Privacy and ethics matter: Choose tools carefully, prioritizing data security and evidence-based approaches over unvetted apps
- Recovery is a journey: Start small, practice self-compassion, expect non-linear progress, and celebrate every moment of presence you create
Research Studies & Resources Referenced
Key Clinical Studies:
- AI in Eating Disorder Care (2025) – Linardon, J., et al. “Using Artificial Intelligence to Advance Eating Disorder Research, Treatment and Practice.” International Journal of Eating Disorders, 58(5):811-812. PubMed: 39921480
- Clinician and Patient Perspectives (2025) – Linardon, J., et al. “Current Practices and Perspectives of Artificial Intelligence in the Clinical Management of Eating Disorders: Insights From Clinicians and Community Participants.” International Journal of Eating Disorders, 58(4):724-734. PMC11969028
- Smartphone Integration (2025) – Linardon, J., et al. “Integrating Artificial Intelligence and Smartphone Technology to Enhance Personalized Assessment and Treatment for Eating Disorders.” International Journal of Eating Disorders. PMC12336790
- Advanced AI Platform (2024) – Monaco, F., et al. “An advanced Artificial Intelligence platform for a personalised treatment of Eating Disorders.” Frontiers in Psychiatry, 15:1414439. Frontiers
- AI Ethical Considerations (2025) – Maas, J., et al. “Artificial Intelligence in Eating Disorder Treatment: A Qualitative Analysis of Clinical Opportunities, Barriers, and Ethical Considerations.” International Journal of Eating Disorders. Wiley
Mindfulness-Based Treatment Research:
- Eating Disorders and AI Promises (2024) – Fitzsimmons-Craft, E.E., Jacobson, N.C. “Eating Disorders Care and the Promises and Pitfalls of Artificial Intelligence.” Missouri Medicine, 121(5):345-349. [PMC11482850](https://pmc.ncbi.nlm.nih.





