You studied 14 hours, got pimped for 20 minutes, and still feel like a fraud. You’re not alone.
It’s 2 AM. You’re reviewing the Krebs cycle for the third time. Your coffee’s cold. Your eyes burn. Tomorrow you’ll present on rounds, and if you don’t know the exact mechanism of every drug your patient is taking, the attending will make sure everyone knows it. You slept four hours last night. Maybe three the night before.
You wanted to save lives. Instead, you’re drowning in yours.
Research spanning multiple studies demonstrates that burnout affects between 45% and 56% of medical students, with rates increasing as students progress through their training. Recent data shows that 87% of entering medical students reported high or very high degrees of impostor phenomenon, with scores increasing significantly by the end of first year.
You’re not broken. You’re surviving a system that treats exhaustion as a rite of passage.
But here’s what nobody tells you during orientation: reclaiming your humanity doesn’t require dropping out, changing specialties, or waiting until residency ends. Sometimes, it starts with 60 seconds between wards.
Let’s explore why you’re burning out before you’ve even started—and how to find your center without leaving medicine.
The Reality: Medicine Selects for Burnout, Then Blames You for It
A systematic review and meta-analysis found that the pooled prevalence of burnout among medical students was 37.23%, with emotional exhaustion peaking after first and third year. Additionally, depersonalization increased early in medical education with minimal regression after development.
Medical students average just 6.5 hours of sleep per night, with 57% reporting poor sleep quality and 33% experiencing excessive daytime sleepiness. Meanwhile, 58.4% of Swedish medical students scored above the clinical threshold for impostor phenomenon.
You’re not imagining the pressure. The data is screaming what you can’t say out loud: medical education is systematically destroying the wellbeing of the people it trains to heal others.
Five Daily Battles You Fight in Silence (And How to Survive Them)
1. The Impostor Spiral: When Your Best Is Never Enough

The Research: Studies show that 87% of entering medical students report high or very high degrees of impostor phenomenon, with women 1.7 times more likely than men to report frequent or intense feelings. Research found that students underrepresented in medicine at predominantly white institutions were 3.0 times more likely to report frequent or intense impostor syndrome compared to those at historically black colleges/universities.
The impostor phenomenon isn’t weakness. It’s a rational response to a system that tells you you’re “excellent” while simultaneously suggesting you’re never quite good enough.
Mindful Solutions:
- The “Impostor Reframe” Script (3 minutes): When impostor thoughts strike, pause. Place your hand on your heart. Breathe. Say aloud: “These feelings don’t mean I’m incompetent. They mean I care about doing well. Every expert was once a beginner. I am exactly where I should be in my training.” Repeat three times. Feel the words in your body, not just your mind.
- Evidence Collection: Keep a “proof folder”—screenshots of good evaluations, patient thank-you notes, peer compliments. When impostor thoughts attack, read three pieces of evidence. Your feelings are valid, but they’re not facts.
- Normalize the Experience: Approximately 30% of medical students and residents identify as impostors, with higher rates among women and international medical graduates. You’re not alone—you’re normal.
Research Reference: Persistent Impostor Phenomenon in Medical Students – Family Medicine
2. Sleep Deprivation as Hazing: When Rest Becomes a Luxury

The Research: Meta-analysis of 109 studies involving 59,427 medical students found that 57% experienced poor sleep quality and 33% reported excessive daytime sleepiness. Medical students sleep an average of 6.5 hours per night—well below the recommended 7-9 hours. Research in Hong Kong showed that 70% of medical students experienced sleep deprivation, with mean nocturnal sleep of only 6.6 hours.
Sleep deprivation doesn’t build character. It impairs judgment, increases medical errors, and predicts burnout.
Mindful Solutions:
- The “Finger Breathing” Reset (60 seconds): Between wards or before a difficult interaction, trace your hand. Breathe in as you trace up your thumb, breathe out as you trace down. Continue around each finger. Five breaths, one per finger. This activates your parasympathetic nervous system and creates a mental reset in under a minute.
- Strategic Napping: If you can find 10-20 minutes between rotations, close your eyes. Even brief rest improves cognitive function. Don’t judge yourself for needing it—embrace it as performance enhancement.
- Non-Negotiable Sleep Hygiene: Protect at least 6.5-7 hours when possible. Turn your phone face-down. Use blackout shades. Sleep isn’t procrastination—it’s how your brain consolidates what you learned today.
Research Reference: Sleep Problems Among Medical Students – Meta-analysis
3. Pimping as Pedagogy: When Public Humiliation Passes for Teaching
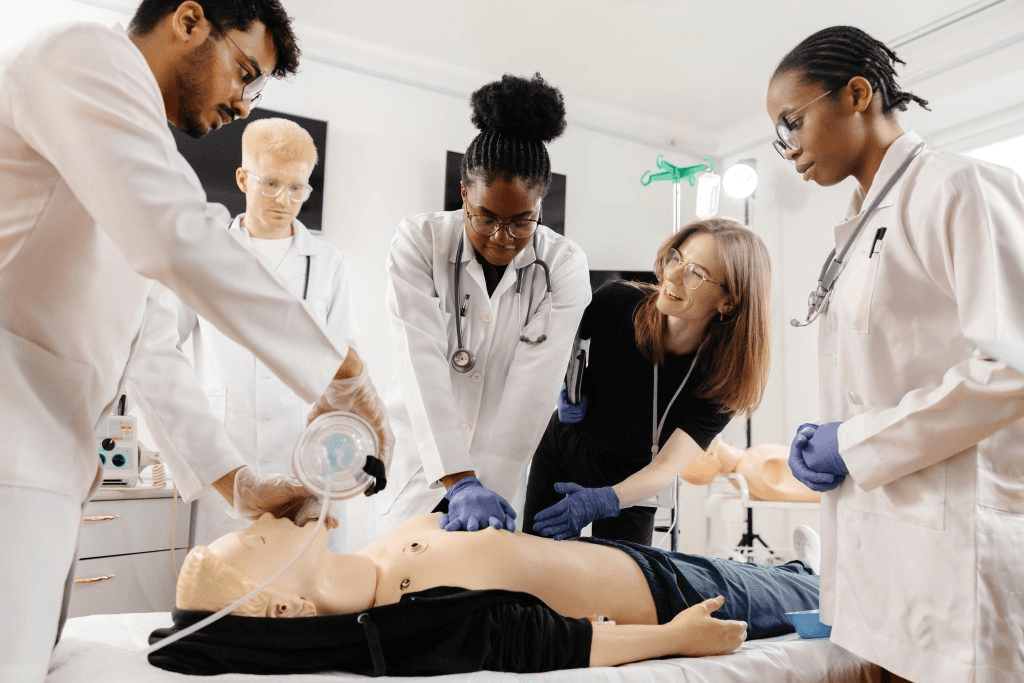
The Research: Research examining learning environments found that medical students in the bottom quartile of learning environment favorability experienced significantly higher rates of burnout, regardless of demographic background. Students who experienced at least one episode of discrimination were significantly more likely to report burnout.
Socratic questioning is valuable. Public humiliation masquerading as education is abuse. Your body knows the difference, even if the system doesn’t.
Mindful Solutions:
- The “I Don’t Know” Power Move: Practice saying “I don’t know, but I’ll look it up and follow up with you.” Say it with confidence, not apology. Not knowing something doesn’t mean you’re stupid—it means you’re a student. That’s literally why you’re there.
- Reframe the Interaction: Remind yourself: “This attending’s behavior reflects their training, not my worth. I can learn from their knowledge without internalizing their delivery.” Separate the information from the emotional delivery.
- Post-Pimping Processing (2 minutes): After a difficult interaction, find a private space. Take three deep breaths. Ask yourself: “What did I actually learn?” Write it down. This reclaims the educational value while releasing the shame.
Research Reference: Learning Environment and Medical Student Burnout – JAMA Network Open
4. The Empathy Paradox: Feeling Everything While Processing Nothing

The Research: Emotional exhaustion in medical students peaks after first year and third year, with moderate improvement after summer breaks and residency match. Studies show that burnout is associated with lower empathy scores, increased depersonalization, and higher rates of depression.
Medical training asks you to feel enough to care, but not so much that you break. Nobody teaches you how to actually do that.
Mindful Solutions:
- The “Compassion for the Patient, Compassion for Self” Practice (90 seconds): After a difficult patient interaction, pause. Breathe. Say silently: “I witnessed their suffering with compassion.” Breathe again. “I cannot carry their suffering for them.” Breathe once more. “I am allowed to feel this and also let it go.”
- Emotional Bookending: Before entering a patient’s room, mentally acknowledge: “I’m entering their story.” After leaving: “I’m stepping out of their story.” This creates psychological containment.
- Find Witness: Identify one trusted peer or mentor. After emotionally heavy cases, share one sentence: “That was hard.” Being seen in your struggle prevents it from becoming trauma.
Research Reference: Temporal Trends in Medical Student Burnout – Family Medicine
5. The Comparison Trap: When Everyone Else’s Highlight Reel Becomes Your Failure
The Research: Research shows that impostor phenomenon scores increased significantly from the beginning to the end of first year medical school. Students with higher impostor scores had significantly lower self-compassion, lower sociability self-esteem, and higher neuroticism and anxiety.
Medical school attracts overachievers, then pits them against each other. The comparison game is designed to make everyone feel inadequate.
Mindful Solutions:
- Social Media Detox: Consider limiting exposure to medical student success stories on social media during high-stress periods. What you’re seeing is curated highlight reels, not reality.
- The “Three Things” Rule: Each evening, write down three things you did today that aligned with why you came to medicine. Talked to a patient kindly. Learned something new. Supported a classmate. These matter more than publications.
- Redefine Success: Your path doesn’t have to look like anyone else’s. Medicine needs researchers AND clinicians, specialists AND generalists, academics AND community physicians. Different isn’t lesser.
Research Reference: Impostor Syndrome Among Medical Students – ScienceDirect
Your Two Essential Quick Resets (That Fit Into Any Clinical Day)
Reset 1: Finger Breathing (60 seconds)
Between wards, before a presentation, or when anxiety spikes:
- Step 1: Hold one hand out, palm facing you.
- Step 2: Use your other hand’s index finger to trace your hand outline.
- Step 3: Breathe IN as you trace up your thumb. Breathe OUT as you trace down.
- Step 4: Continue around all five fingers.
- Result: Five complete breaths, grounding presence, activated parasympathetic nervous system.
This works because it combines tactile sensation, controlled breathing, and counting—three things that interrupt the stress response. It’s discrete enough to do anywhere.
Reset 2: The “Impostor Reframe” Script (3 minutes)
When impostor thoughts attack (before exams, after mistakes, during evaluations):
- Minute 1: Place your hand on your heart. Feel it beating. Ground yourself in physical reality.
- Minute 2: Say aloud (or in your mind): “These doubts are common. They don’t mean I’m incompetent. They mean I care about doing well. Every attending I admire was once exactly where I am now.”
- Minute 3: Take three deep breaths. With each exhale, consciously release one specific impostor thought. “I release the belief that I’m the dumbest person here. I release the fear that I’m going to fail. I release the idea that I don’t deserve to be here.”
This practice doesn’t eliminate impostor syndrome—it changes your relationship with it.
The Bigger Picture: You Deserve Better Than “This Is Just How It Is”
Let’s be brutally honest: you shouldn’t need these coping strategies. You deserve systemic changes—protected sleep hours, mental health support without stigma, learning environments free from mistreatment, and a culture that values wellbeing alongside excellence.
Recent research demonstrates that improving learning environment quality significantly reduces burnout rates. Studies show that medical schools implementing wellness curricula, mental health screening, and anti-discrimination policies see measurable improvements in student wellbeing.
Advocate for change. Join wellness committees. Speak up about mistreatment. Support classmates experiencing burnout. Your individual resilience practices are survival tools, not acceptance of broken systems.
But while you’re fighting for change—and you should be—you also need tools to survive tomorrow’s rounds.
The Truth You Already Know But Keep Forgetting
You chose medicine because you wanted to help people. You still do—you just forgot that includes helping yourself.
Burnout isn’t the price of becoming a good doctor. It’s what happens when a system mistakes exhaustion for dedication. But here’s the paradox: the more you protect your humanity, the better physician you’ll become.
That 60-second breathing practice? It’s not wasted study time. It’s how you stay present for your patients instead of going through the motions. It’s the difference between surviving medical school and thriving beyond it.
Your Tomorrow Starts Right Now
Right now, before you go back to studying, try this:
Hold one hand out. Trace your fingers while you breathe. Five breaths. One minute.
Ask yourself one question: “What do I need right now to feel okay?”
Not what your attending needs. Not what your classmates are doing. What YOU need.
Maybe it’s calling a friend. Maybe it’s taking a walk. Maybe it’s permission to close your books and sleep.
Whatever it is, give yourself that thing. Even if imperfectly. Even if briefly.
Tomorrow, the exams will still come. The rounds will still happen. The pressure will still exist.
But you? You’ll be a little more grounded.
Because you chose presence over perfection. Because you chose breath over burnout. Because you chose you.
Resources That Actually Help
- AAMC Medical Student Well-Being Resources: Evidence-based strategies and institutional guidelines – students-residents.aamc.org/medical-student-well-being
- Student National Medical Association (SNMA): Support specifically for underrepresented students – snma.org
- Physician Support Line: Anonymous, confidential peer support – physiciansupportline.com
- HeadSpace for Healthcare Workers: Free meditation and mindfulness app
- The Happy MD: Evidence-based physician burnout prevention – thehappymd.com
The Final Question
The exams will still come. The patients will still need you. The training will continue.
But if you don’t protect your humanity, none of it matters.
One minute. That’s all it takes to remember who you are beneath the white coat.
The question isn’t whether you have time.
The question is: Can you afford not to?






